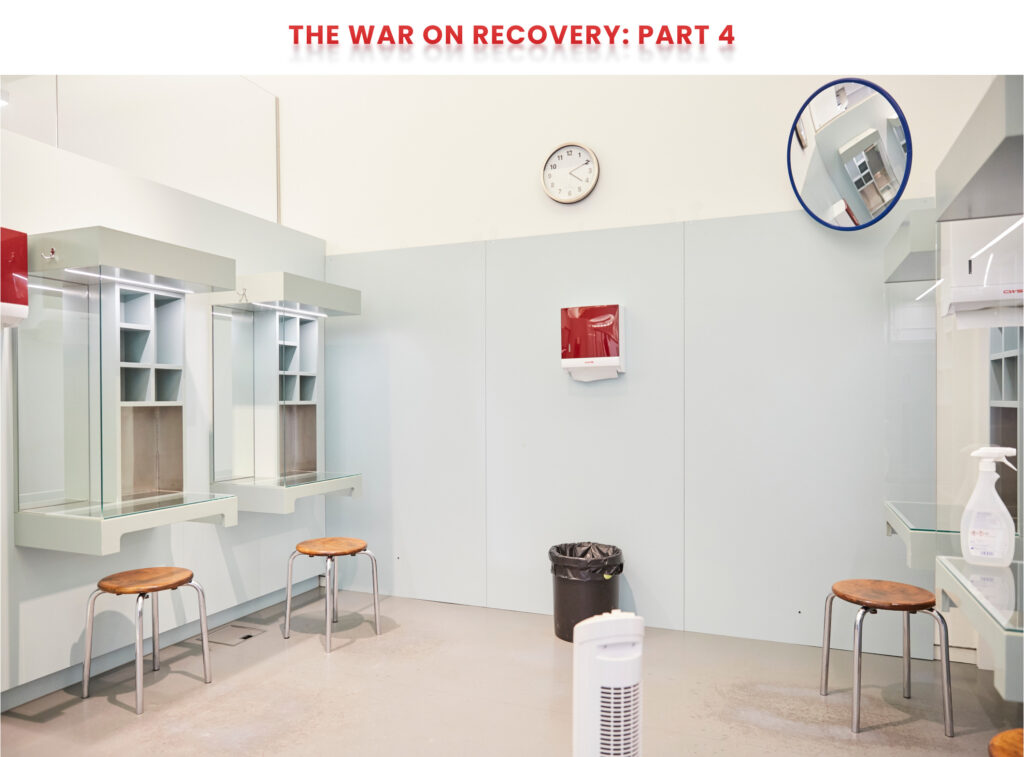
ZURICH — The lobby of this addiction clinic is unremarkable, really, except for the network of metal chutes and tubes that hug the walls as they snake downward from a pharmacy on the upper floors. Every few minutes, a new prescription comes clattering down, delivering a bottle full of powerful and effective pills used to treat opioid addiction to a waiting patient at the front desk. Sometimes, it’s methadone. Other patients prefer slow-release morphine. In rare cases, for those at high risk of overdose or infectious disease, this clinic even prescribes pharmaceutical-grade heroin.
This scene is typical of a Monday afternoon in Switzerland. But in the United States, where opioid addiction medications remain controversial and highly stigmatized, it would be unthinkable. Just two medications are approved to treat opioid withdrawal symptoms in the U.S., and methadone, the more effective of the two, is kept under lock and key. Doctors cannot prescribe it except at specialized clinics. Pharmacies cannot dispense it. Instead, most patients seeking methadone treatment must attend their clinic each morning to receive a single dose.
But at Arud Centre for Addiction Medicine, a leading Swiss clinic, all patients in need of addiction care are given instant access to weeks’ worth of medication. They are not required to participate in counseling, or subjected to drug tests, or punished if they relapse and use illicit substances. It is a strategy that many American methadone clinics warn would result in disaster — but that European experts say is the continent’s key to success.
“We have access to a very broad population because it’s so easy to access our treatment center,” Philip Bruggmann, a Swiss doctor and Arud’s head of internal medicine, told STAT during a recent visit to the clinic’s headquarters in central Zurich. “This wouldn’t be possible in a system which is very restrictive, where people are getting kicked out of the program or disappearing because they can’t comply with the regulations and rules. I think we would lose a lot of patients. They would die.”
Instead, the opioid death rate here is roughly one-twentieth the rate in the United States. The country has become a model for a highly effective, evidence-based policy response to a drug epidemic. And in roughly a dozen wealthy, developed nations where methadone is far more accessible than in the U.S., public health outcomes are far better. Residents of Germany, Australia, France, the United Kingdom, and the Netherlands all can legally obtain methadone far more easily than in the United States. Each country has lower rates of opioid overdose, infectious disease transmission, and death.


The Swiss model serves as a noteworthy counterexample to the American system, where methadone and other medications used to treat opioid addiction are guarded by a maze of laws and regulations and typically viewed with skepticism or judgment.
Shaken by the nation’s jarring rate of opioid overdose deaths — over 80,000 per year — American doctors, lawmakers, and public health officials have begun to advocate for liberalizing access to methadone. Methadone, they argue, is the best tool available to address the crisis: Those who take it are 59% less likely to die of opioid overdose.
American methadone clinics, however, argue that the current restrictions are necessary safety precautions. Methadone is itself an opioid sometimes used to treat pain, and can cause sedation or even overdose when misused or taken in combination with alcohol and other drugs. The presence of fentanyl in the U.S. drug supply has made patient care even more complex and, according to some clinics, more dangerous. Prescribing opioid-based addiction medications more liberally, they argue, would result in increased overdoses, higher crime, and even cause people to become addicted to opioids after using methadone they obtained on the black market.
Addiction experts in Europe disagree.
“There’s just no evidence for it,” Bruggmann said. “It really helps people to reintegrate, to stabilize, and I’m not aware of a single case of a person who became opioid-dependent because of this treatment. If you leave it to the black market, people disappear and you can’t reach them, and I think the risk is much bigger.”

‘I’m really free’
Andi Hüttenmoser, 62, has seen firsthand how much access to addiction care has improved in Switzerland over the last three decades.
One of Arud’s original patients, Hüttenmoser has spent much of the last four decades on an up-and-down journey between drug use and recovery. In the mid-1980s, he was addicted to heroin, had been infected with hepatitis C, and was suffering from liver cirrhosis. But the clinic, and its policy of treating patients no matter their circumstance, helped him stabilize.
Hüttenmoser began by taking methadone, but later switched to slow-release morphine tablets because methadone made him sweat. In 2014, he also became one of the first hepatitis C patients in Switzerland to be fully cured using advanced new antivirals.
He has been sober, and hepatitis C-negative, since then. And for the last five years, Hüttenmoser has worked as one of Arud’s peer support coaches — serving, he said, as a “bridge between the institution and the consumer.”
The clinic’s approach to addiction treatment, he said, makes recovery in Switzerland far easier than in the United States. Decisions at Arud are made after a conversation between a patient and doctor: By and large, patients have the power to choose whichever addiction medication they feel will work best for them.
Those who choose methadone, slow-release morphine, or buprenorphine, another common drug used to treat opioid addiction, can receive up to 30 days of medication at once. Methadone is available in pill form — a significant difference from U.S. methadone clinics, which offer liquid medication, making it more difficult to take home or transport.
Those receiving prescription heroin — a far smaller population — can receive the drug either in injectable or tablet form. The measure is only offered to patients whose drug use is most dangerous: Those at least 18 years of age who have suffered from opioid addiction for at least two years and have failed at least two attempts at treatment using more conventional medications. The clinic even offers a small room where people are permitted to inject the drug, formally known as diacetylmorphine, under medical supervision, though they’re not permitted to inject drugs they bought on the black market.
Though the approach may appear extreme, Swiss clinical trials have shown patients offered prescription heroin have high treatment retention rates, and many eventually transition to medications that don’t induce the same euphoric effect, like methadone or slow-release morphine. Following Switzerland’s success, countries including Germany, the United Kingdom, and the Netherlands have also adopted the approach. And since the Covid-19 pandemic, many Swiss patients on heroin-assisted treatment have even been allowed to receive a week of take-home doses — meaning that prescription heroin in Switzerland is, in many cases, less tightly regulated than prescription methadone in the United States.
While Arud strongly cautions against the continued use of illicit substances, it does not mandate drug testing as a condition of receiving medication. Nor, unlike many U.S. clinics, does it mandate counseling sessions: Each of the patients Hüttenmoser helps independently chose to see a therapist or counselor.
“The bar to access treatment is so much lower, and it’s not chaos. People are getting really good care.”
Honora Englander, U.S. physician studying access to addiction care in France
The clinic also goes to great lengths to ensure that pregnant women with opioid addiction continue receiving medications like methadone — it would be “very dangerous” for them not to, Bruggmann said. The policy is a stark contrast from typical practice in many U.S. health care settings, where providers and youth welfare agencies often force women to choose between keeping their baby and remaining in treatment using methadone or buprenorphine, even as doctors caution that cutting off medication treatment could lead to outcomes disastrous for both mother and child, like overdose or death.
“You can get as much as you think you need,” Hüttenmoser said of the clinic’s attitude toward medication. As a result, he added, Swiss addiction patients enjoy autonomy and quality of life that would be unimaginable across the Atlantic.
“I’m really free,” he said. “I can do what I want. I can go [for] two months in another country. It’s no problem.”
The same is true elsewhere on the continent. Countries across Europe prioritize patient convenience over strict regulation, said Honora Englander, an American physician currently studying access to addiction care while in France as part of a Fulbright scholarship. As a result, she said, patients generally find care simpler and easier, and as a result are far less likely to experience drug-related health issues like overdose, HIV, or hepatitis.
“The work of being a patient in France is far less,” she said. “Instead of traveling daily to [a methadone clinic], patients can — even relatively early in treatment — get several weeks of methadone at a time from their local community pharmacy. The bar to access treatment is so much lower, and it’s not chaos. People are getting really good care.”

‘It’s better to give them methadone’
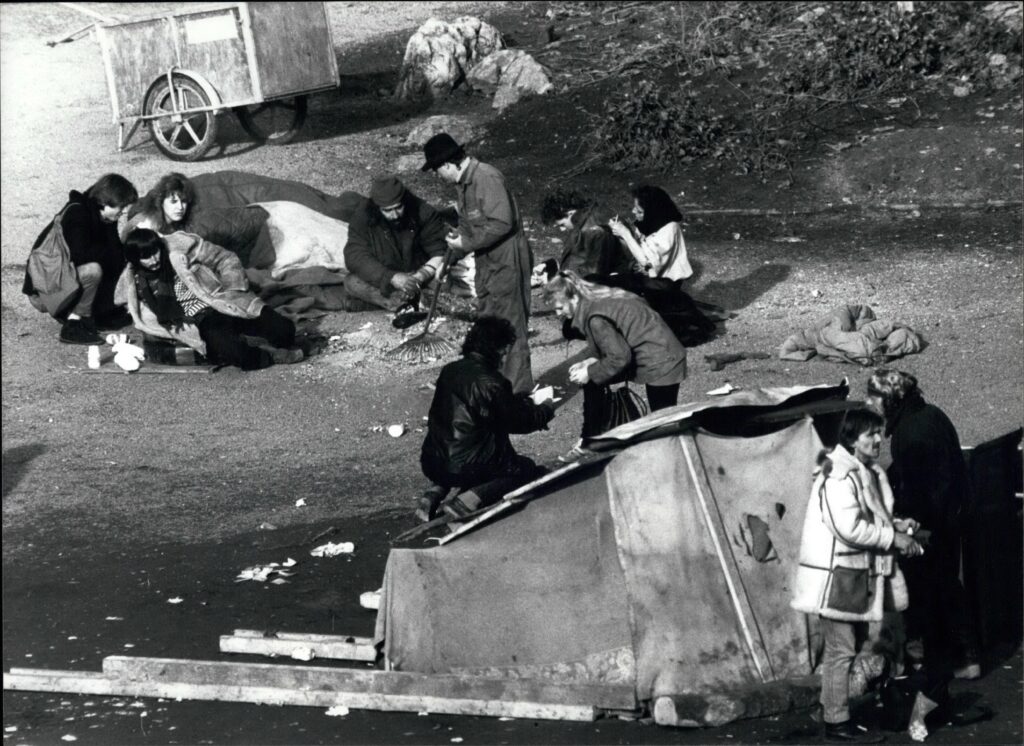
Methadone treatment was once controversial in Switzerland, too. Three decades ago, the country experienced a reckoning on drug use not unlike the debate unfolding in the United States. At one point, the country’s HIV transmission and AIDS death rates were the highest in Western Europe. Its overdose rate was three times higher than it is today.
In response, Swiss lawmakers took on an age-old debate: drug policy based on treatment, or drug policy based on law enforcement.
In the end, they chose a multipronged plan that placed a heavy emphasis on treatment and harm reduction — in particular, easy access to clinics that offered addiction medications like methadone and buprenorphine. In less than a decade, enrollment in methadone treatment climbed from zero to 18,000.
At the time, many viewed the approach as radical — especially in Switzerland, a generally conservative country where women only gained the right to vote in 1971. But many Swiss now see the move as obvious, and as an unmitigated success. Between the early 1990s and early 2000s, expanded access to medication and harm-reduction services like syringe exchange and supervised consumption sent rates of drug overdose, HIV, and hepatitis C plummeting.
Nowhere is the change more evident than at Platzspitz, a large city park just blocks from Arud that sits directly across from Zurich’s bustling central train station. In the late 1980s, the station became a drug-dealing hub, and Platzspitz was such a haven for heroin use that it became known as “Needle Park.”
On a sunny afternoon, park-goers played chess on Platzspitz’s pristine grass, their bare feet making clear they no longer feared the stab of a stray syringe. The same is true across Switzerland: Low-barrier access to methadone, buprenorphine, slow-release morphine, and sometimes prescription heroin has helped wind down the country’s drug epidemic, saving thousands from disease or death and all but eliminating visible drug use in public spaces.
Some debate remains about more aggressive tactics like prescription heroin and supervised consumption sites, but Switzerland’s drug policy doctrine has not been seriously challenged since 1997, when 71% of voters rejected a referendum that would have significantly curtailed methadone treatment, syringe exchange, and supervised consumption rooms.
Switzerland’s experience has largely ended debate among Western and Central European public health experts regarding methadone access.
“In all the European Union member states, methadone treatment is working quite well,” Ingo Ilja Michels, a longtime drug policy official who has worked across Europe and Asia and served as the head of Germany’s Office of the Federal Drug Commissioner, said in an interview. “I don’t know any state in the world that has seen failure in this regard.”
Germany, too, was once restrictive with methadone, requiring that patients who enrolled in medication treatment programs pledge to be abstinent and enroll in counseling. Eventually, however, most policymakers there concluded that restricting the medication only to patients who were already stable was doing more harm than good.
“Yes, of course it’s better” for patients to receive medication coupled with counseling and other support services, Michels said. “But it’s better to give them methadone than nothing.”
Requiring patients to be fully abstinent and compliant with too many restrictions is “not realistic,” he added. “Even the right-wing politicians in the Bundestag now are saying: It’s better to give them methadone than to ask them to stay abstinent.”

But in the U.S., ‘we don’t have that’
Few American experts dispute Europe’s relative success in combating drug addiction and helping people who use drugs to stay healthy.
But some defenders of the American approach to addiction treatment argue that other countries’ situations are fundamentally different, and that policy solutions employed elsewhere would be either riskier or less effective if employed in the United States. They point out that some European countries offer cautionary tales, not success stories: In the United Kingdom, methadone deaths spiked in the 1990s, forcing the country to institute safeguards such as requiring some patients to take methadone daily at a community pharmacy.
“It’s very difficult to equate the experiences of other countries to our country,” said Mark Parrino, the founder and president of the American Association for the Treatment of Opioid Dependence, a national advocacy group that represents methadone clinics. “They have different backgrounds. They have different finances. Basically, the French government provides funding — all of it. We don’t have that here.”
The U.S. overdose crisis does have stark differences from past European drug epidemics. Most European nations have some form of universal health insurance, making issues of cost and payment for addiction care far simpler.
In North America, the illicit drug market is also dominated by fentanyl, the ultra-potent synthetic opioid that now causes a large majority of American overdose deaths. Fentanyl, to date, has not been detected in large quantities in Europe, meaning that opioid addiction there is typically easier to treat.
American addiction doctors, however, argue that the fentanyl epidemic gives all the more reason to expand methadone access. People using fentanyl are far more likely to die of an overdose from illicit substances, making the need to treat them with a comparatively weak, pharmaceutical-grade medication all the more urgent. Moreover, they argue, those addicted to fentanyl have developed extraordinarily high tolerances for opioids — meaning that any overdose risk associated with methadone treatment is negligible compared to the overdose risk of continued fentanyl use.
Treatment and harm reduction are also far more unpopular among Americans than Europeans. In the U.S., tactics like supervised consumption and prescription heroin, while now commonplace in Switzerland, are political nonstarters. Even less controversial practices like syringe exchange or the use of test strips to check illicit drugs for fentanyl or xylazine — a veterinary sedative often known as “tranq” — still face political resistance in some U.S. cities and states.
Yet there is little evidence that Europe’s flexible approach is having adverse public health effects.
“In America, you can’t expect this. If you’re on the street, you’re on the street. Nobody cares.”
Andi Hüttenmoser, peer support coach at Arud Centre for Addiction Medicine
“There are stunning differences in terms of treatment access, and there are stunning differences in terms of overdose rates,” Englander said, adding that patients in France “are getting their methadone from community pharmacies, and France is not seeing an epidemic of methadone overdose.”
In the U.S., attitudes appear to be shifting — at least among addiction doctors and policymakers. On Capitol Hill, Sen. Ed Markey (D-Mass.) and a coalition of Democratic and Republican lawmakers have introduced legislation that would allow trained addiction doctors to prescribe methadone, and pharmacies to dispense it.
Nora Volkow, the director of the National Institute on Drug Abuse, announced for the first time in 2022 that she believed physicians should be able to prescribe methadone directly to patients. More recently, she told STAT she believes that if the U.S. allowed universal access to methadone and buprenorphine, opioid deaths would fall by 50%, if not more.
The Biden administration has a stated goal of making addiction medication available to anyone who wants it by 2025, much as many European countries do now. But realizing that vision would require structural changes ranging from providing the medications in jails and prisons to vastly increasing reimbursement rates for doctors hoping to treat addiction.
Perhaps the biggest change, however, would be one of attitude — and the channeling of compassion toward people who use drugs.
“In America, you can’t expect this,” Hüttenmoser said. “If you’re on the street, you’re on the street. Nobody cares. This is a big difference between the Americans and Swiss, or Europe.”
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies. Our financial supporters are not involved in any decisions about our journalism.
To submit a correction request, please visit our Contact Us page.





STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect